2021.10.01
Changes in the treatment of venomous snake bites in Japan (from Dr. Atsushi Sakai)
In Japan, venomous snake bites are caused by four species of habu (habu, himehabu, saxima habu, and tokara habu) and two Japanese pit vipers, but it is the largest habu and Japanese pit vipers that cause the most damage and problems, and treatment has been focused on these two species. Today, bites by the Formosan habu, which escaped and settled in Japan after being imported, and the Japanese mountain lionfish, which was once thought to be a non-poisonous snake, are also a problem. In 1984, the Tsushima pit viper bite from Tsushima Island, Nagasaki Prefecture, which was considered a different species from the Japanese pit viper, was also added to the list. Antivenin sera are inseparable from the treatment of snake bites, and changes in treatment are also changes in the use of antivenin, but another inseparable factor is cephalanthin. Figure 1 Figure 2
Habu bite
In the Okinawa and Amami regions, habu bites have long been a serious problem that deeply affects people’s lives, and even in 1980, about 400 people were bitten and several died each year. Even in 1980, about 400 people were bitten and several people died each year. By 2020, the number of bites had decreased to about 60 due to extermination and various improvements in the living environment, and the use of antitoxins has prevented deaths.
In 1895, an antitoxin serum made by immunizing horses was used for treatment, and its effectiveness was confirmed. In Japan, the Infectious Disease Research Institute (later to become the Institute of Medical Science), headed by Shibasaburo Kitasato, used this method to immunize people with habu venom from Amami-Oshima Island to create a prototype antitoxin, which was developed into the habu antitoxin in 1904. In the early days, a mixed serum of habu and pit viper was produced. Habu venom was also used. In 1905, 118 patients in Okinawa and Amami were treated with serotherapy, and although 5 of them died, this was 1/3 of the number without serotherapy, which was considered quite effective. Even in the 1960s, it was often administered around the injured area.
However, the antitoxin is not the only way to treat the disease. In those days, transportation was not convenient and it took quite a long time to reach medical facilities, and antitoxin was in liquid form and could not be stored in rural areas where electricity was not available. After 1956, Yoshio Sawai and his colleagues at the Institute of Medical Science, University of Tokyo, began research on purification, partial digestion, and freeze-drying of antiserum, which led to the development of lyophilized antitoxin (1959), improving its efficacy and shelf life. The development of lyophilized antitoxin (1959) improved its efficacy and shelf life, making treatment with antitoxin possible even in remote areas, and the fatality rate dropped to 1%. In addition, unit price sera for habu and pit viper began to be produced in 1961 and 1963, respectively.
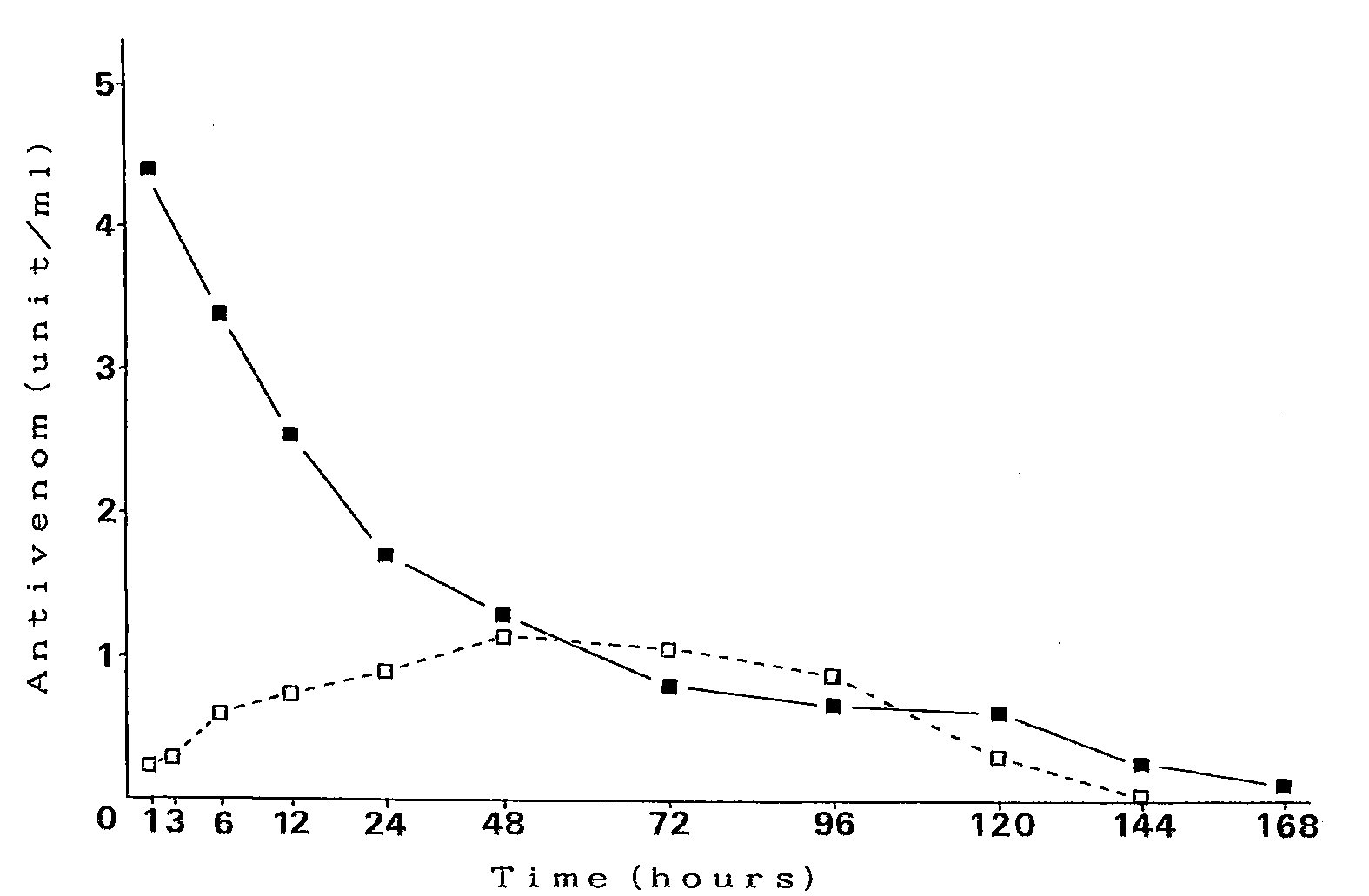
Early antitoxins contained inactive proteins unrelated to the antibody, and these were separated and purified to produce antitoxins with only the gammaglobulin fraction of the antibody portion. The removal of impurities reduces side reactions. Furthermore, pepsin digestion separates IgG, which has a molecular weight of about 150,000, into F(ab’)2, which has a molecular weight of about 110,000 for the antigen-binding portion, and the Fc region. n speed is faster. In muscular injection, IgG is also absorbed slowly and has a long half-life of 25 days, while F(ab’)2 has high tissue permeability and a short half-life of 9 days. Horse antibodies are of course foreign to humans, and the longer they are in the body, the more antibodies to horse antibodies are produced, and adverse reactions are more likely to occur with repeated administration. Incidentally, in the United States, the antitoxin CroFab (Crotalidae polyvalent immune fab), which is a Fab with a molecular weight of 50,000 after papain digestion, is currently being produced. (Fig. 1) The half-life is even shorter at 15 to 23 hours.
Apart from antitoxins, Kagoshima has been inoculating residents in some areas with habu toxoids since 1970 to reduce the severity of bites. However, its effectiveness has not been very clear. Today, the vaccination of toxoid is no longer performed since 2002, as the improvement of medical institutions and the emergency transportation system have made it possible to receive treatment in a short time.
In addition, EDTA solution (chelating agent) was used for local cleansing, inotropic drugs, adrenaline, and dextrose Ringer’s solution were administered. Since snake venom could be detected in the leachate at the site of injury, small incisions were sometimes made in the fang scar area and aspirated continuously with an aspirator if the patient came to the hospital within a short time. Because the protein in snake venom is a metalloprotein, and chelating agents also suppress its activity, the bite site was incised and washed with EDTA. Some physicians also washed the site with tetracycline at the same time. The astringent action of tannic acid, used as a protein precipitant, was used for first aid cleaning because it also neutralizes habu venom. Studies have shown that tannic acid extracted from astringent persimmons has a higher neutralizing power than local tannic acid, and first aid kits containing this tannic acid solution were sold by the Society of Tropical Medicine. Cephalantin, which is still commonly used in the treatment of pit viper bites, was initially used in the treatment of hub bites, and studies on its effectiveness were reported, but since 1990 it has rarely been seen and is no longer used in treatment.
Although broad-spectrum antibiotics are administered to prevent infection, some report that they are unnecessary because there have been no reports of infections from snakebite as well as hubbites. In addition, tetanus toxoid is generally administered for animal bites, but there have been no reports of tetanus in hubbites. There have been few reports of animal bites causing tetanus, including overseas, with only a few reports of cases following venomous snake bites in Nigeria and Thailand.
Compartment syndrome is a problem in hub bites because the swelling is so severe. Therefore, a decompression incision is made, but because the hub’s tusks are 1~2 cm long and venom may be injected intramuscularly, a fasciotomy and cleaning is performed.
Mamushi bites(esp. the mamushi, Gloydius blomhoffi)
Local treatment used to involve bonding and making several incisions for aspiration and drainage, but this is no longer done because the incisions increase the length of treatment time. Since the swelling is not as severe as that of a habu bite, a decompression incision has not been used very often for a long time. However, pit viper bites often involve the fingers of the hand, which are peripheral and may cause circulatory disturbance due to swelling, so a decompression incision is sometimes used to avoid compartment syndrome. Prior to 1990, peripheral veins were incised, aspirated, and debrided with an antihypertensive bandage. This was recommended because immediately after the injury (within 15 minutes), compression and squeezing would shorten treatment days. In many cases, however, it is difficult to provide treatment within 30 minutes of injury.
Local cleaning with drugs has also been used since around 1950, as in the case of hub bites. In many cases, after incision, the wound was cleaned with 1% potassium permanganate solution, but its effectiveness was not clear, so isodine solution was used to disinfect the wound.
In the 1950s, however, intravenous cephalantin was reported to speed up the resolution of swelling, suppress hemolysis, and shorten the number of treatment days.
Because pit viper bites have a low mortality rate and tissue damage such as necrosis is less severe than in hub bites, there is little demand for unit price pit viper antitoxin, and initially a mixed serum of hub and pit viper was produced.
Cephalanthin is an alkaloid extracted from a plant. Residents in Taiwan used extracts of the plant to treat venomous snake bites, and Shuji Hasegawa, then director of the Institute of Infectious Diseases at the University of Tokyo, and others began using it to treat habu and pit viper bites after reports of its hemolytic and lethal effects on snake venom. Like habu antitoxin, pit viper antitoxin was still in liquid form and difficult to store in remote areas, and the complications of anaphylaxis and serum sickness discouraged the use of sera. Subsequently, antitoxin became available in dried formulations and also in more purified formulations. However, in the 1970s and 1980s, many studies were reported comparing the efficacy of antitoxins and cephalanthin in treatment. The results showed that there was not much difference in their effectiveness, but that cephalantin was sufficient for treatment because cephalantin had no side effects and antitoxins had side effect problems. From the reports of these studies, the use of antitoxins was considerably discouraged until about 1990.
However, the reports of these studies are very inadequate as comparative studies. Many of the reports simply stated that the antitoxin was administered, but did not specify the method or time of administration. One report, comparing 114 cases over a 10-year period beginning in 1978, described the administration of antitoxin as subcutaneous, intramuscular, or intravenous, with no discussion of differences in route of administration. There is no explanation in the package insert of the antitoxin as to which method of administration is best. This is because it has long been unrecognized that there is a significant difference in efficacy depending on the route of administration. Nevertheless, the report states that the antitoxin is effective if administered within 3 hours. Because of side-effect problems, antitoxin was administered subcutaneously or intramuscularly in a significant number of cases until about 1990. Furthermore, because it is difficult to diagnose whether or not a patient is seriously ill within a short period of time after injury, the antitoxin was administered in a less effective manner after some degree of observation and after symptoms had progressed, clearly not taking advantage of the effects of the antitoxin.
Therefore, we used ELISA in animal experiments to examine changes in local and blood levels of residual venom after intramuscular administration of pit viper venom, as well as changes in residual venom levels after intramuscular or intravenous injection of the antitoxin 30 minutes after venom administration. The results showed that the amount of residual toxin in the blood as well as in the local area was clearly reduced in the case of intravenous injection of the antitoxin. Since the 1990s, the use of intravenous antitoxin has gradually increased and many cases have been treated with intravenous infusion. (Figure 2) A report from Myanmar examines the efficacy of intramuscular injection of antitoxin. This is because there is no staff available to administer intravenous injections in remote areas, and in areas with many highly toxic snakes, life cannot be saved without administering antitoxin. This was the same situation in Japan in the past. However, no other country seems to have questioned the effectiveness of antitoxin. Intravenous administration of antitoxin neutralizes the poison in the blood in a short time and can prevent serious illness to a great extent. However, the spread of the swelling does not stop immediately because the local toxin does not immediately decrease to zero. Therefore, it was sometimes thought to be not very effective. However, in pit viper bites, where venom is injected into the blood vessels and platelets drop below 10,000 in a short time, platelet counts recover in a short time after intravenous infusion of antitoxin. These cases show how effective the antitoxin is.
Although cephalantin is still in considerable use today, Sawai et al. reported in 1988 that cephalantin was not effective in suppressing pit viper venom in an in vitro study. Of course, cephalantin does not directly suppress the action of the venom, so its effectiveness can hardly be determined by measuring differences in lethality, hemorrhage, and necrosis in mice. However, there is nothing wrong with using it in clinical practice, as some have suggested that it seems to speed up recovery time, and there are no side effects to worry about. However, it is important to realize that it is only to be used as an adjunct and not as a substitute for antitoxins.
Cephalantin was originally used for chemotherapy of tuberculosis, and Hasegawa Shuji is well known as its originator. In 1949, Hasegawa Shuji became the director of the Institute of Medical Science of the University of Tokyo (then known as the Research Institute of Infectious Diseases), and in 1952, Sawai Yoshio became the head of the laboratory at the institute, where he developed a prototype of an antitoxin serum. Shuji Hasegawa also served as the first president of Gunma University and as the president of the Japan Institute of Snake Research, while Yoshio Sawai became a board member at the same time and was appointed president in 1973. It is very interesting that these two men belonged to the same Institute of Medical Science of the University of Tokyo and the Japan Serpent Research Institute, yet they showed completely opposite results.
Antivenoms specifically bind to snake venom and suppress its effects, and are undoubtedly very effective, but they also carry the risk of anaphylaxis, so antihistamines and steroids are now recommended in advance, although studies have shown that this method can reliably prevent anaphylaxis. In any case, adrenaline and a ventilator should always be prepared when administering antitoxin, since there are no reports of anaphylaxis, and some overseas studies have shown that preadministration of adrenaline considerably reduces the incidence of anaphylaxis.
There are also reports that plasma exchange has been effective, but the number of cases is small and the effect has not been clearly demonstrated. Hemodialysis (HD) was the main treatment for acute renal failure before 2000, but after 2000, continuous hemodiafiltration (CHF) or hemodiafiltration dialysis (HDF) has been used, and in recent years, continuous hemodiafiltration dialysis has increased. Because acute renal failure is rare in hub bites, dialysis and other procedures are not often performed. In recent years, hyperbaric oxygen therapy has been used in severe cases to improve circulatory disturbance and hypoxia, to improve peripheral circulation, and to reduce tissue swelling by increasing the amount of oxygen in the body.
Yamakagashi bite
The first report of a case of Natrix tigrinus snakebite in a 49-year-old man in 1931 (1932) was a relatively serious case with transient hemorrhagic predisposition. 10 minutes later, he had a severe headache, but it was transient and resolved. A tendency to hemorrhage was observed, and the coagulation time was markedly prolonged to 47 minutes on the second day of the disease. Brown urine and hematuria due to hemolysis were also seen, typical of mountain lion bites still seen today, but no treatment was described. A second case was reported in 1932, but the details are unknown. Twenty years later, in 1953, a third case was reported, in which a 10-month-old boy was bitten and showed bleeding tendency, with a clotting time of 45 minutes, and in this case, blood transfusion, Ringer’s solution, and oil penicillin were administered. The patient gradually became mildly ill and was discharged 7 days later.The fourth case report of an 11-year-old boy in 1968 was the first to describe fibrinogen levels, which had decreased to 60 mg/dl on the third sick day, and fibrinolytic activity was also increased. Treatment included penicillin, antihistamine, intravenous epsilon (hemostatic), and fibrinogen infusion, and the patient was discharged on the 26th day.
There were very few reports in medical journals, and the fact that the mountain lion was a venomous snake was not widely known, even among medical professionals. In 1971, DIC was first diagnosed in a 61-year-old man. Fibrinogen was less than 20 mg/dl and platelets were decreased to 55,000. Treatment included 4,000 ml exchange transfusions, heparinization of blood, and hemodialysis, followed by heparin, fibrinogen, transamine (to treat bleeding tendency), and calcicol (calcium supplement), and the coagulation system values recovered, but there was no urination and a 10-day renal biopsy revealed extensive bleeding and Two months later, he died of pulmonary edema, the first reported death from a porcupine bite.
We began studying mountain oak toxin around 1980, but prior to that there was only one report (1976) on mountain oak toxin, which claimed that it activates factor X. In our experiments, intravenous injection into mice showed strong toxicity, but subcutaneous and intramuscular injections were about 1/20 of the toxicity. It caused systemic hemorrhage, and fibrin thrombi were observed in pulmonary capillaries and renal glomeruli. It was also shown to have strong blood coagulation activity and activation of prothrombin. 1984 death of a junior high school student due to intracerebral hemorrhage after he was bitten by a mountain lion by hand led to the development of prototype antitoxins by immunizing rabbits in 1986 and goats in 1987. This antitoxin was used in 11 cases, and in 10 cases where it was administered (intravenous infusion) by 4 days after the injury, the bleeding stopped within a short time after administration and the patients showed remarkable recovery, even though they had significant coagulopathy and DIC. In one case, administered 6 days after the injury, the patient had already developed acute renal failure, so dialysis was performed, and it took nearly one month for the patient to recover. In 2000, an antitoxin was produced by immunizing horses with a research funded by the Ministry of Health, Labour and Welfare of Japan, and all cases in which the antitoxin was administered by 3 days after the injury recovered within a few days without complications of acute renal failure. However, four fatal cases of cerebral hemorrhage occurred within a few days.
The action of mountain lion venom is almost exclusively procoagulant and does not directly damage tissues like hub or pit viper venom. Therefore, when the toxin is neutralized in the blood by administration of antitoxin in a short time, the consumption of coagulation factors is stopped. Since the coagulation factors continue to be replenished, they begin to increase rapidly as the poison ceases to act, and the bleeding tendency improves within a short period of time. The short and pronounced effect of the antitoxin is characteristic of mountain lionfish bites.
In treatment, heparin and gabexate mesylate are administered in cases diagnosed as hypofibrinogenemia or DIC. In our animal studies, heparin improves coagulation abnormalities to some extent. However, the use of heparin is contraindicated in venomous snake bites, which have a strong tendency to hemorrhage due to their strong coagulant effect. The efficacy of gabexate mesylate, which is used in the treatment of DIC, is not clear in the treatment of snakebite wounds. Plasma exchange has been used in some cases, but the effect is less pronounced, and in one case the bleeding tendency did not improve even after three plasma exchanges and rapidly improved with administration of antitoxin. Fibrinogen replacement without administration of antitoxin is also not recommended because it promotes clot formation.
In highly toxic venomous snakebites, serotherapy is the mainstay of treatment, but the time to administration and the method of administration are very important. In addition, because the venom composition differs from snake to snake, different venom injection sites and venom doses cause different pathologies, and many viper bites cause bleeding tendency and acute renal failure, but the pathogenesis mechanism differs from snake to snake, so clarification of venom action is very important for appropriate treatment.
Reference data
Kobayashi Teruyuki “Viper” Bunshun Bunko 2000
Hifumi T, Sakai A, Kondo Y, et al: Venomous snake bites: clinical diagnosis and treatment. J Intensive Care 3:16, 2015, DOI 10.1186/s40560-015-0081-8
Figure 1: IgG antibodies
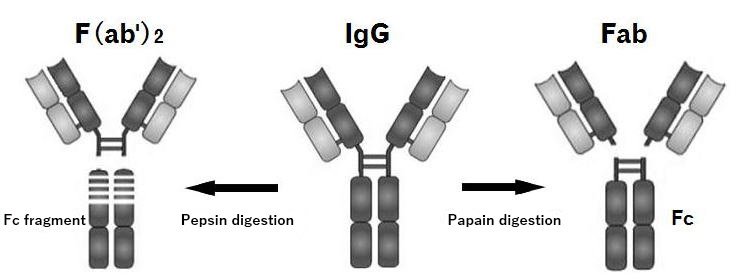
Figure 2. Changes in blood levels of antibodies in rabbits.
Amount of antibody when only antibody was injected intravenously(■) and intramuscularly(□)