As a local treatment, several incisions were made for aspiration and evacuation, but this is no longer widely used because the incisions require more time for treatment. Since the swelling is not as severe as in the case of a hub bite, incisions to reduce swelling have not been used for a long time. In Mamushi bites, however, the fingers are often injured and the peripheral location of the injury can cause circulation problems due to swelling. In order to avoid compartment syndrome, a decompression incision is sometimes performed. This varies considerably from institution to institution, and some perform decompression incisions at a relatively early stage.
Before 1990, peripheral veins were incised, aspirated, and de-vascularized by applying a tourniquet. This was recommended because the days of treatment could be shortened by compression and squeezing immediately after the injury (within 15 minutes). In many cases, however, it is difficult to provide treatment within 30 minutes of injury.
As with hub bites, local cleansing with chemicals has also been used since around 1950. In many cases, the incision was cleaned with 1% potassium permanganate solution, but the effect was not clear, so isodine solution was used to disinfect the wound.
Until about 1960, antitoxin was the main systemic treatment, but in the 1950s, intravenous cepharanthine was reported to speed up the disappearance of swelling, suppress hemolysis, and shorten the duration of treatment.
Since the mortality rate of Mamushi bites is low and the tissue damage, such as necrosis, is less severe than that of habe bites, the demand for Mmushi antivenom per unit price is low, and a mixed serum of habe and pit viper was initially produced. Cephalanthin, an alkaloid extracted from a plant, was used to treat venomous snake bites by residents in Taiwan, and was used in the treatment of hub and Mamushi bites by Shuji Hasegawa, Director of the Institute of Infectious Diseases at the University of Tokyo, and others, based on reports of the hemolytic and lethal effects of snake venom.
Like the habu antivenom, the Mamushi antivenom was still in liquid form, making it difficult to store in remote areas, and the complications of anaphylaxis and serum sickness discouraged the use of the serum. Later, the antivenom came in dried form and also in more purified form. However, in the 1970s and 1980s, many studies comparing the efficacy of antivenom and cepharanthine in treatment were reported. The results showed that there was not much difference in their efficacy, but that cepharanthine was sufficient for treatment, because cepharanthine had no side effects and antitoxin had problems with side effects. From these research reports, the use of antitoxins was considerably discouraged until about 1990.
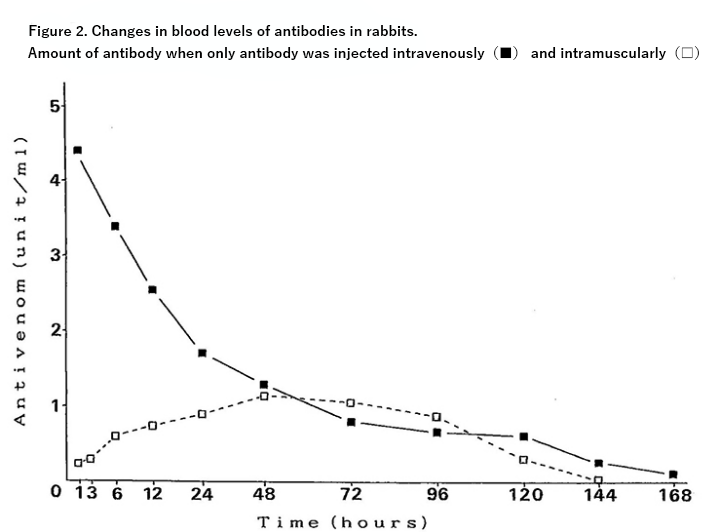
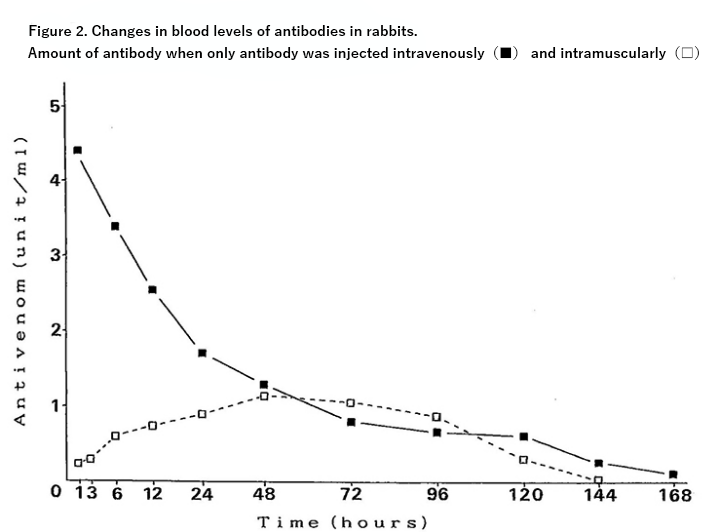
However, the reports of these studies are very inadequate as comparative studies. Many of the reports merely stated that the antitoxin was administered, but did not specify the method or time of administration. One report, comparing 114 cases over a 10-year period starting in 1978, stated that the antitoxin was administered subcutaneously, intramuscularly, or intravenously, and did not discuss differences in the route of administration. The antitoxin package insert does not explain which route of administration is preferred. This is because it has not been recognized for a long time that there is a significant difference in efficacy depending on the route of administration. Nevertheless, the report states that the antitoxin is effective if it is administered within 3 hours. Because of the side effects, antitoxin was administered subcutaneously or intramuscularly in a significant number of cases until about 1990. Furthermore, because it is difficult to diagnose whether a patient will become severely ill in a short time after injury, antitoxin was administered in a less effective way after the symptoms had progressed, after a certain amount of observation, and the effect of antitoxin was obviously not utilized.

Therefore, we investigated the changes in the amount of residual venom in the local and blood after intramuscular administration of pit viper venom using ELISA in animal experiments, and also investigated the changes in the amount of residual venom when antitoxin was injected intramuscularly or intravenously 30 minutes after venom administration. The results showed that the intravenous antitoxin clearly reduced the amount of residual venom in the blood as well as in the local area. Since the 1990s, the use of intravenous antitoxin has gradually increased, and many cases have been treated with intravenous infusion. (Since the 1990s, the use of intravenous antitoxin has gradually increased and many cases have been treated with intravenous infusion. (Fig. 2) There is a report on the effectiveness of intramuscular injection of antitoxin in Myanmar. This is because there are no staff who can give intravenous injections in remote areas, and in areas where there are many highly toxic snakes, antitoxin must be administered to save lives. This is the same situation that existed in Japan in the past. However, no other country seems to have doubts about the effectiveness of antitoxin. Intravenous injection of antitoxin can neutralize the poison in the blood in a short time and prevent serious illness to a great extent. However, the local venom does not immediately go to zero, and the swelling does not immediately stop spreading. Therefore, it was sometimes thought to be not very effective. However, in cases of pit viper bites, where the venom is injected into the blood vessels and the platelet count drops to less than 10,000 in a short time, the platelet count recovers in a short time after intravenous infusion of antitoxin. Such cases show how effective the antitoxin is.
Although cepharanthine is still used quite a bit, Sawai et al. reported in 1988 that cepharanthine was not effective in suppressing pit viper venom in an in vitro study. Of course, since cepharanthine does not directly suppress the action of the venom, the effect can hardly be judged by measuring the difference in lethality, bleeding, and necrosis in mice. However, there is nothing wrong with using it, as some clinical studies have shown that it seems to speed up recovery time, and there are no side effects to worry about. However, it should be noted that it is used as an adjunct and not as a substitute for antivenom.
Cepharanthine was originally used for chemotherapy of tuberculosis, and Shuji Hasegawa is famous as its founder. Hasegawa served as the director of the Institute of Medical Science of the University of Tokyo (then known as the Research Institute of Infectious Diseases) from 1949, and in 1952, Sawai Yoshio became the head of the Laboratory of Testing and Manufacturing at the same institute, where he developed a prototype antivenom serum. At the same time, Yoshio Sawai became a member of the board of directors, and in 1973, he was appointed chairman of the board. It is very interesting that these two men belonged to the same Institute of Medical Science of the University of Tokyo and the Japan Serpentine Research Institute, but showed completely contrary results.
The antivenom specifically binds to the snake venom and suppresses its action, which is undoubtedly very effective, but because of the risk of anaphylaxis, it is now recommended to administer antihistamine and steroids in advance. However, there are some overseas studies that show that adrenaline preadministration significantly reduces the incidence of anaphylaxis, so in any case, adrenaline and a ventilator must be prepared when administering antitoxin.
Plasma exchange has also been reported to be effective, but the number of cases is small and no clear effect has been shown. Hemodialysis (HD) was the main treatment for acute renal failure before 2000, but since 2000, continuous hemodiafiltration (CHF) or hemodiafiltration dialysis (HDF) has been used, and in recent years, continuous hemodiafiltration dialysis has been increasingly used. In recent years, continuous hemodiafiltration has been increasingly used. Habe bites rarely cause acute renal failure, so dialysis is not often used. In recent years, hyperbaric oxygen therapy has been used to improve the condition of severe cases by increasing the amount of oxygen in the body to improve circulatory disturbance and hypoxia in the body, improve peripheral circulation, and reduce tissue swelling.
Reference data
Kobayashi Teruyuki “Viper” Bunshun Bunko 2000
Hifumi T, Sakai A, Kondo Y, et al: Venomous snake bites: clinical diagnosis and treatment. J Intensive Care 3:16, 2015, DOI 10.1186/s40560-015-0081-8
Blog Published on Oct 01, 2021 Changes in the treatment of venomous snake bites in Japan (from Dr. Atsushi Sakai)