The first report of a case of Yamakagashi bite in a 49-year-old man in 1931 was “a relatively severe case of Yamakagashi (Natrix tigrinus) snakebite with temporary hemorrhagic predisposition” (1932). Hemorrhagic tendency was observed, and the clotting time was markedly prolonged to 47 minutes on the second sick day. Brown urine and hematuria due to hemolysis were also observed. This is a typical porcupine bite wound that is still seen today, but there is no mention of any treatment. A second case was reported in 1932, but the details are unknown. Twenty years later, in 1953, a third case was reported. A 10-month-old boy was bitten and showed a tendency to bleed, with a clotting time of 45 minutes. In this case, blood transfusion, Ringer’s solution, and oily penicillin were administered. The patient gradually got better and was discharged after 7 days. 1968 was the fourth report of an 11-year-old boy, in which the fibrinogen level was described for the first time, and it had decreased to 60 mg/dl on the third sick day, and the fibrinolytic activity was also increased. Treatment included penicillin, antihistamine, intravenous epsilon (for hemostasis), and fibrinogen infusion, and the patient was discharged on the 26th sick day.
There were very few reports in medical journals, and it was not widely known to the medical profession that the mountain lion was a poisonous snake. The first case of DIC was diagnosed in a 61-year-old man in 1971. In 1971, DIC was first diagnosed in a 61-year-old man with fibrinogen below 20 mg/dl and platelets down to 55,000. Treatment included exchange transfusion of 4,000 ml of blood, heparinization of blood, hemodialysis, and subsequent administration of heparin, fibrinogen, transamin (to treat bleeding tendency), calcicol (calcium supplement), etc. Coagulation system values recovered, but there was no urination, and renal biopsy on the 10th day showed extensive bleeding and necrosis. Two months later, the patient died of pulmonary edema, and is reported as the first fatal case of mountain goat bite.
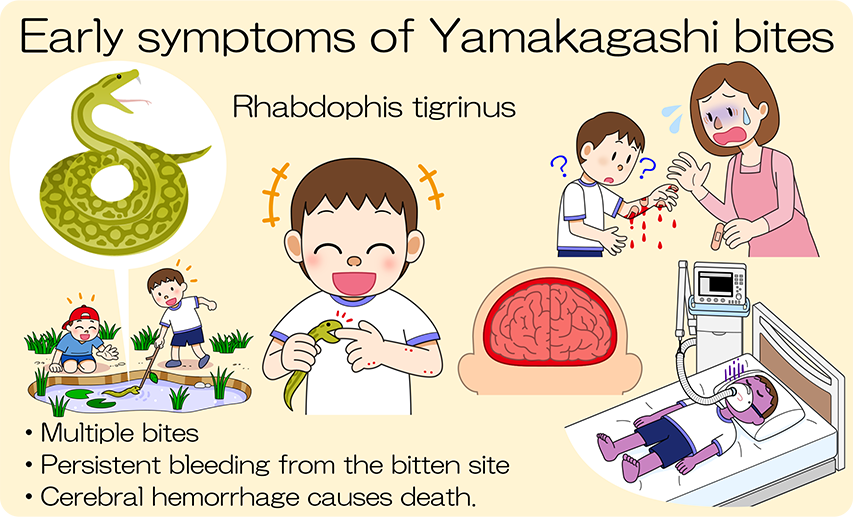
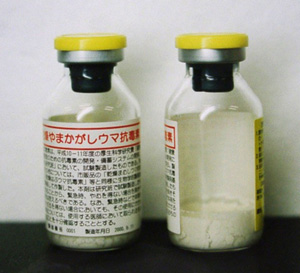
We began research on mountain squirrel venom around 1980, but prior to that, there was only one report on mountain squirrel venom (1976), which stated that it activates factor X. In our experiments, intravenous injection into mice showed strong toxicity, but subcutaneous and intramuscular injection showed about 1/20 of the toxicity. In our experiments, intravenous injection into mice showed strong toxicity, but subcutaneous and intramuscular injections were about 1/20th as toxic. It has caused systemic bleeding, and fibrin thrombi have been observed in pulmonary capillaries and renal glomeruli. In 1984, a junior high school student was bitten by a porcupine and died from intracerebral hemorrhage, which led to the development of a prototype antitoxin by immunizing rabbits in 1986 and goats in 1987. This antivenom was used in 11 cases, and in 10 cases administered (intravenous infusion) up to 4 days after injury, the bleeding stopped within a short time after administration, showing remarkable recovery, despite the fact that the patients had marked coagulopathy and DIC. One case administered 6 days after the injury was already suffering from acute renal failure, so dialysis was performed and it took almost a month to recover. Later, in 2000, an antitoxin was produced by immunizing horses under the auspices of the Ministry of Health, Labor and Welfare’s National Institute of Health Sciences. All the patients who received the antitoxin by 3 days after the injury recovered within a few days without acute renal failure. However, four of the fatal cases developed cerebral hemorrhage within a few days.

The action of Yamakagashi venom is almost exclusively blood coagulation-promoting, and it does not directly damage tissues as do habu and Mamushi venoms. Therefore, when the venom in the blood is neutralized in a short time by the administration of antitoxin, the consumption of coagulation factors is stopped. As the clotting factors continue to be replenished, they begin to increase rapidly as the venom ceases to act, and the bleeding tendency improves in a short time. It is characteristic of mountain ash bites that the effect of the antitoxin is pronounced in a short time.
In the treatment of patients diagnosed with hypofibrinogenemia or DIC, heparin and gabexate mesylate have been administered. In our animal studies, heparin has shown some improvement in coagulation abnormalities. However, the use of heparin is contraindicated in cases of viper bites, which have a strong coagulant effect and tendency to bleed.
In addition, the gabexate mesylate effect used in the treatment of DIC is not clear in the treatment of bite wounds. In some cases, plasma exchange has been used, but the effect was not very remarkable. In some cases, the bleeding tendency did not improve even after three plasma exchanges, and it rapidly improved after administration of antitoxin. Fibrinogen supplementation without antitoxin administration is not recommended because it promotes thrombus formation.
Reference data
Kobayashi Teruyuki “Viper” Bunshun Bunko 2000
Hifumi T, Sakai A, Kondo Y, et al: Venomous snake bites: clinical diagnosis and treatment. J Intensive Care 3:16, 2015, DOI 10.1186/s40560-015-0081-8
Blog Published on Oct 01, 2021 Changes in the treatment of venomous snake bites in Japan (from Dr. Atsushi Sakai)